We set out for Roanoke, VA on Monday and arrived in Jacksonville
at 5:30pm. Still 1100 miles, no matter what route you take.

A night shot of 81 South in Virginia.
I will visit my cardiologist next Tuesday - Inauguration Day.
I am unsure what I will find out, but I hope to find out that I am improving.
I may not know my ejection fraction (EF) until February - that will be three full months of treatment. It is important to me to find out that my ejection fraction (previously 10%, should be 50-70%) has improved before returning to work. My chances of heart failure remain high while my ejection fraction is low. If the EJ does not increase, my cardiologist has suggested a defibrillator or pacemaker.



Everyone keeps telling me...One step at a time.
WHAT IS A DEFIBRILLATOR?
Defibrillation is the definitive treatment for the life-threatening cardiac irregularities. Defibrillation consists of delivering a therapeutic dose of electrical energy to the affected heart with a device called a defibrillator. This depolarizes a critical mass of the heart muscle, terminates the arrhythmia, and allows normal rhythm to be reestablished by the body's natural pacemaker, in the sinoatrial node of the heart.
Defibrillators can be external, transvenous, or implanted, depending on the type of device used. Some external units, known as automated external defibrillators (AEDs), automate the diagnosis of treatable rhythms.
An implantable cardioverter defibrillator (ICD) is a small device that's placed in your chest or abdomen. This device uses electrical pulses or shocks to help control life-threatening, irregular heartbeats, especially those that could lead the heart to suddenly stop beating (sudden cardiac arrest). If the heart stops beating, blood stops flowing to the brain and other vital organs. This usually causes death if it's not treated in minutes.
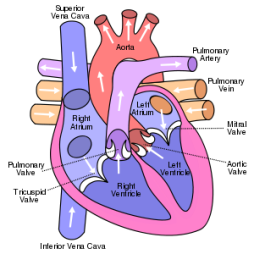
A problem with any part of the electrical system process can cause irregular heartbeats called arrhythmias (ah-RITH-me-ahs). During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. Faulty electrical signaling in the heart causes arrhythmias.
ICDs use electrical pulses or shocks to treat life-threatening arrhythmias that occur in the ventricles (lower chambers of the heart).
When these ventricular arrhythmias occur, the heart can't effectively pump blood, and a person will pass out within seconds and die within minutes if not treated. To prevent death, the condition must be treated right away with an electric shock to the heart. This treatment is called defibrillation.
An ICD has wires with electrodes on the ends that connect to the chambers of your heart. The ICD will continually monitor your heart rhythm. When the device detects that you're having an irregular rhythm in your ventricles, the ICD will use low-energy electrical pulses to restore a normal rhythm. If this doesn't restore your normal heart rhythm, or if your ventricles start to quiver rather than contract strongly, the ICD will switch to high-energy electrical pulses for defibrillation.
Doctors also treat irregular heartbeats with another device called a pacemaker. An ICD is similar to a pacemaker, but there are some differences. Pacemakers can only give off low-energy electrical pulses. They are often used to treat less dangerous heart rhythms, such as those that occur in the upper chambers of your heart. Most new ICDs can act as both pacemakers and ICDs.
Comparison of a Defibrillator and a Pacemaker

The illustration compares an implantable cardioverter defibrillator and a pacemaker.
Figure A shows the location and general size of an implantable cardiac defibrillator in the upper chest. The wires with electrodes on the ends are inserted into the heart through a vein in the upper chest. Figure B shows the location and general size of a double-electrode pacemaker in the upper chest. The wires with electrodes on the ends are inserted into the heart through a vein in the upper chest.

A photo showing an implanted pacemaker.
WHAT IS A PACEMAKER?
A pacemaker is a small device that's placed under the skin of your chest or abdomen to help control abnormal heart rhythms. This device uses electrical pulses to prompt the heart to beat at a normal rate.
Pacemakers are used to treat heart rhythms that are too slow, fast, or irregular. These abnormal heart rhythms are called arrhythmias (ah-RITH-me-ahs). Pacemakers can relieve some symptoms related to arrhythmias, such as fatigue (tiredness) and fainting. A pacemaker can help a person who has an abnormal heart rhythm resume a more active lifestyle.
Information from the National Heart Lung and Blood Institute
www.nhlbi.nih.gov





.svg.png)
